Overview
Acute acalculous cholecystitis (AAC) represents inflammation of the gallbladder in the absence of demonstrated calculi (see the image below). The disease process of AAC is distinct from that of the calculous variety, in which the primary initiating event is believed to be obstruction of the cystic duct. Acalculous cholecystitis typically occurs as a secondary event in patients who are hospitalized and are acutely ill with another disease.
The diagnosis often is difficult and is often delayed because of comorbidities that decrease sensitivity and specificity of clinical and imaging evaluation. A high degree of suspicion is required on the part of the physician. A much higher rate of complications is observed in patients with acalculous cholecystitis (eg, gangrene, perforation) because of the more fulminant course and coexistent disease. As a result, some authors propose the term necrotizing cholecystitis to reflect the fact that acalculous cholecystitis does not simply represent cholecystitis without stones.
Emphysematous cholecystitis, which can occur as a complication of acute cholecystitis, is seen in the images below.
 Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall.
Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall. 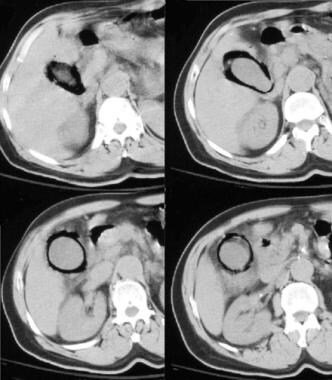 CT images of emphysematous cholecystitis.
CT images of emphysematous cholecystitis. Preferred examination
Early imaging evaluation is required for patients with acalculous cholecystitis, and frequently, multiple diagnostic tests are performed. No single imaging study is ideal. The 3 primary imaging modalities often are complementary, with ultrasonography (US) or computed tomography (CT) scanning providing anatomic information and evaluation of adjacent structures and cholescintigraphy providing functional information. US and cholescintigraphy should be the initial imaging tests performed to evaluate possible AAC. CT scanning is preferred if other diseases in the differential diagnosis are more likely or if CT scanning needs to be performed for another indication.
Limitations of techniques
All available modalities have a significant false-positive and false-negative rate and generally are better at excluding, rather than confirming, the presence of acalculous cholecystitis.
Although it is unusual for acalculous cholecystitis to occur in patients with a normal gallbladder, on US and cholescintigraphy examinations, the gallbladder may be found to be normal early in the course of the disease. For patients who continue to experience clinical deterioration and for whom clinical evaluation is not possible or fails to demonstrate an alternative source, many authors recommend maintaining a low threshold for instituting empiric, minimally invasive therapy in the form of percutaneous cholecystostomy.
Radiography
Plain film radiography is of limited use in the diagnosis of acute acalculous cholecystitis (AAC). Emphysematous cholecystitis (seen in the image below) may occur as a complication of acute cholecystitis; more than one half of such cases occur in the setting of acalculous disease. This form of complicated cholecystitis typically is seen in older male patients with diabetes.
 Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall.
Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall. On upright abdominal radiographs, AAC may be evinced by the presence of an air-fluid level in the right upper quadrant; such a finding represents gas in the gallbladder lumen. The presence of intramural gas is indicated by findings of a curvilinear gas collection that conforms to the gallbladder wall. Gas is visualized only in more severe cases on plain film. US and CT scanning are much more useful.
The presence of gas is often associated with gangrene and perforation.
Computed Tomography
CT scanning often is performed as the diagnostic examination of choice in patients presenting with abdominal pain in the critical care setting or in patients with fever or leukocytosis of undefined etiology. CT scanning offers the advantage of evaluating the entire chest and abdomen; it has the disadvantage of requiring transport to the scanner. One should be familiar with the CT scan signs that suggest acalculous cholecystitis in the appropriate clinical setting (see the image below).
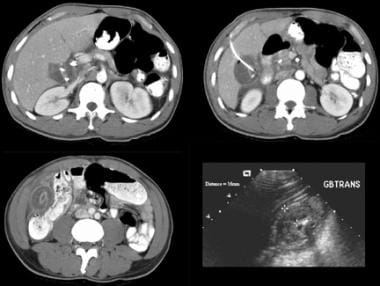 Despite drainage, this patient continued to experience right upper quadrant pain and leukocytosis. Ultrasonographic and CT scan studies demonstrate transhepatic cholecystomy catheter in good position, but interval development of markedly worsening gallbladder wall edema and pericholecystic inflammatory changes have occurred. At surgery, gangrenous gallbladder was found and resected successfully.
Despite drainage, this patient continued to experience right upper quadrant pain and leukocytosis. Ultrasonographic and CT scan studies demonstrate transhepatic cholecystomy catheter in good position, but interval development of markedly worsening gallbladder wall edema and pericholecystic inflammatory changes have occurred. At surgery, gangrenous gallbladder was found and resected successfully. The normal gallbladder wall is barely perceptible as a thin enhancing rim on contrast-enhanced CT scans. In the absence of gallstones, imaging relies on ancillary findings of cholecystitis.
CT scan findings in patients with acute acalculous cholecystitis (AAC) are as follows:
- Gallbladder wall thickening
- Mucosal irregularity
- Luminal distension
- Increased bile density (biliary sludge)
- Intramural or intraluminal gas
- Intraluminal hemorrhage
- Localized pericholecystic fluid collections
- Inflammatory infiltration of pericholecystic fat (see the image below)
- Indistinctness of the liver-gallbladder interface
 Despite drainage, this patient continued to experience right upper quadrant pain and leukocytosis. Ultrasonographic and CT scan studies demonstrate transhepatic cholecystomy catheter in good position, but interval development of markedly worsening gallbladder wall edema and pericholecystic inflammatory changes have occurred. At surgery, gangrenous gallbladder was found and resected successfully.
Despite drainage, this patient continued to experience right upper quadrant pain and leukocytosis. Ultrasonographic and CT scan studies demonstrate transhepatic cholecystomy catheter in good position, but interval development of markedly worsening gallbladder wall edema and pericholecystic inflammatory changes have occurred. At surgery, gangrenous gallbladder was found and resected successfully.
The diagnosis of AAC with CT scanning requires that 2 major diagnostic criteria be met or, alternatively, that 1 major criterion and 2 minor criteria be met.
The major criteria are as follows (see also the video below):
- Gallbladder wall thickening greater than 3 mm
- Subserosal halo (ie, gallbladder wall edema)
- Pericholecystic fatty inflammation
- Pericholecystic fluid (without ascites or hypoalbuminemia)
- Mucosal sloughing
- Intramural gas
CT cine loop of acalculous cholecystitis demonstrates irregular gallbladder wall, pericholecystic inflammation, and perihepatitis in gallbladder fossa. Necrotic gallbladder was present at surgery.
The minor criteria consist of the following:
- Gallbladder distension (>5 cm transverse)
- High-attenuation bile (sludge)
Degree of confidence
Although mucosal sloughing and intramural gas are specific findings, they are observed infrequently. Isolated local pericholecystic fluid collections and pericholecystic inflammatory changes are relatively specific and suggest advanced disease, but they lose specificity in the setting of ascites, recent abdominal surgery, or anasarca.
Reported sensitivity and specificity vary but generally have been greater than 90-95%. As with other imaging modalities, the specificity of many of these findings is decreased in the typical populations at risk for acalculous cholecystitis because of comorbid conditions, such as recent surgery or trauma, multisystemic organ failure, ascites, or hypoalbuminemia.
Ultrasonography
Usually, US is the first examination performed in cases of possible acalculous cholecystitis. This modality has the advantages of being readily available, portable to the bedside, and able to identify other, adjacent pathologies. Primary disadvantages of US include the high incidence of nonspecific abnormal examinations and the inability to survey the entire abdomen.
The normal gallbladder has sonolucent bile and a thin wall; no localized pain is present. Ultrasonographic signs compatible with acalculous cholecystitis include the following (see also the images below):
- Gallbladder wall thickening
- Ultrasonographically localized tenderness over the gallbladder
- Subserosal edema
- Pericholecystic fluid
- Gallbladder distension
- Biliary sludge
- The presence of gas
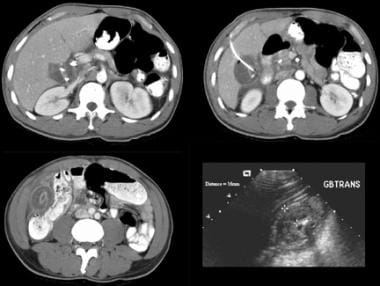
 Ultrasonograms of ICU patient with fever of unclear etiology. Ultrasonographic findings of acalculous cholecystitis include marked gallbladder wall thickening and pericholecystic fluid. Localized tenderness could not be evaluated.
Ultrasonograms of ICU patient with fever of unclear etiology. Ultrasonographic findings of acalculous cholecystitis include marked gallbladder wall thickening and pericholecystic fluid. Localized tenderness could not be evaluated. 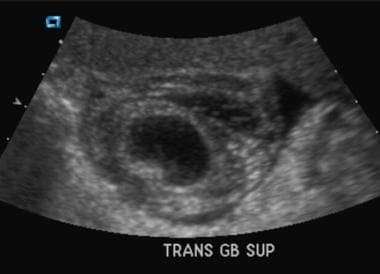 Transverse ultrasonogram demonstrates marked gallbladder wall thickening and pericholecystic fluid collection in a patient with AIDS who was managed conservatively. No localized tenderness was noted, and hepato-iminodiacetic acid scan demonstrated delayed filling but otherwise was normal. Patient recovered with treatment of underlying pneumonia, and ultrasonographic findings normalized within 2 weeks.
Transverse ultrasonogram demonstrates marked gallbladder wall thickening and pericholecystic fluid collection in a patient with AIDS who was managed conservatively. No localized tenderness was noted, and hepato-iminodiacetic acid scan demonstrated delayed filling but otherwise was normal. Patient recovered with treatment of underlying pneumonia, and ultrasonographic findings normalized within 2 weeks. 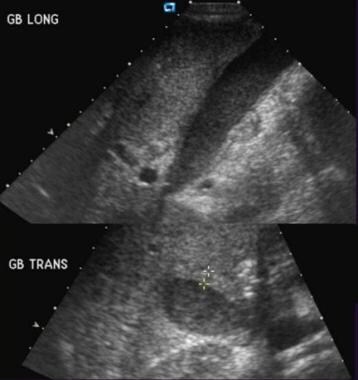 A 53-year-old man status post–endoscopic stenting for pancreatic cancer with progressive fever, leukocytosis, and right upper quadrant pain. Ultrasonogram demonstrates gallbladder distension, biliary sludge, borderline wall thickness, and localized tenderness consistent with acalculous cholecystitis.
A 53-year-old man status post–endoscopic stenting for pancreatic cancer with progressive fever, leukocytosis, and right upper quadrant pain. Ultrasonogram demonstrates gallbladder distension, biliary sludge, borderline wall thickness, and localized tenderness consistent with acalculous cholecystitis.
Failure of the gallbladder to contract after the infusion of cholecystokinin has been reported as an additional criterion, but the response often is too variable to be of use in these patients.
The diagnosis of acute acalculous cholecystitis (AAC) with US requires that 2 major diagnostic criteria be met or, alternatively, that 1 major criterion and 2 minor criteria be met.
The major criteria are as follows:
- Gallbladder wall thickening greater than 3 mm
- Striated gallbladder (ie, gallbladder wall edema)
- Ultrasonographic Murphy sign (ie, localized gallbladder tenderness)
- Pericholecystic fluid (without ascites or hypoalbuminemia)
- Mucosal sloughing
- Intramural gas
Minor criteria consist of the following:
- Gallbladder distension (>5 cm transverse)
- Echogenic bile (sludge)
Gallbladder wall thickness should be measured in the transverse plane, provided the gallbladder has not collapsed. The presence of ascites or decreased oncotic pressure (as occurs in patients with hypoalbuminemia) confuses the finding, unless the finding is markedly discordant. Similarly, the presence of pericholecystic fluid is not meaningful in the presence of generalized ascites.
However, the occurrence of pericholecystic fluid as a localized finding often signifies advanced disease or perforation. The Murphy sign is the most specific ultrasonographic finding, but often it cannot be evaluated because of the patient's clinical condition.
Degree of confidence
The reported sensitivity and specificity of US in the evaluation of acalculous cholecystitis vary from 23-95% and 40-95%, respectively. This degree of variance occurs because of differences in patient populations, clinical courses, and imaging technologies employed over time. The sensitivity and specificity are greater than 90% in the subset of patients with acalculous cholecystitis who present in the outpatient setting.
Overall, the sensitivity and specificity approach 70%. As the proportion of patients in the critical care environment increases, the diagnostic accuracy decreases.
Several studies have documented a high incidence of abnormal gallbladder ultrasonograms in the ICU environment in asymptomatic patients who were not suspected of having acalculous cholecystitis. At least 1 abnormal finding was seen in 50-85% of patients in this setting; 3 abnormal findings were seen in as many as 57% of patients. None of these patients had localized gallbladder tenderness by US.
Serial US has been of benefit in some studies; the fact that the appearance on short-term follow-up images progressively worsens increases the specificity for diagnosis.
Nuclear Imaging
Hepatobiliary scintigraphy (HBS) is a physiologic test that evaluates hepatic bile formation, excretion, and ductal functional patency.
Imaging typically is performed with dynamic image acquisition for up to 4 hours following the intravenous (IV) administration of 5 mCi of a technetium-99m ( Tc) – labeled iminodiacetic acid derivative. Peak liver uptake is at 5-10 minutes, with subsequent gallbladder visualization by 20 minutes and duodenal visualization by 30 minutes (see the videos below).
Normal hepato-iminodiacetic acid scan. Prompt hepatic concentration of radiopharmaceutical is noted, along with early visualization of the gallbladder and drainage into the duodenum.
Hepato-iminodiacetic acid scan of acalculous cholecystitis. Prompt uptake of radiopharmaceutical is noted in the liver, along with drainage into the bowel without gallbladder visualization by 90 minutes.
If nonvisualization or questionable visualization of the gallbladder occurs but adequate hepatic uptake and excretion into the bowel are seen, IV morphine sulfate (0.04 mg/kg) may be administered at 30-40 minutes, with imaging carried out for up to 1 hour. This raises intrabiliary pressure by inducing contraction of the sphincter of Oddi and filling of the gallbladder, provided the cystic duct remains patent. A lateral view may be helpful if a question remains concerning gallbladder filling; the gallbladder is located anteriorly in this projection.
Some have attempted to improve accuracy by pretreating the patient with cholecystokinin infusion before performing HBS, so as to empty the distended gallbladder. HBS may be nondiagnostic in patients with liver failure and intrahepatic cholestasis of any cause because of the inability to conjugate and excrete the radiotracer.
Additional useful findings on cholescintigraphy include the presence of an area of increased pericholecystic radiotracer accumulation in the gallbladder fossa. This rim sign is associated with complications such as gangrene. Radiotracer extravasation rarely may be visualized in the setting of perforated gangrenous cholecystitis if the cystic duct remains patent.
Degree of confidence
HBS is accurate in the diagnosis of calculous cholecystitis because the primary event is believed to be cystic duct obstruction. In cases of acalculous cholecystitis, functional obstruction usually occurs in the disease process but is variable and is not the primary process. Not surprisingly, the sensitivity and specificity of HBS are decreased in this setting.
In general, diagnostic quality studies with augmentation yield a sensitivity of 80-90% and a specificity of 90-100%.
False positives/negatives
The false-positive rate without pharmacologic augmentation is as high as 40% in some series, decreasing the specificity of the test. With morphine augmentation, the false-positive rate is decreased and the specificity is improved.
False-negative results (gallbladder filling in the presence of acalculous cholecystitis) also may occur. Early filling of the gallbladder (within the first 30 min) excludes the diagnosis of acalculous cholecystitis, but with delayed filling after augmentation, the false-negative rate may be as high as 20%.
J David Lane, MD, RT Chief, CMH Vascular and Interventional Radiology, Wisconsin Radiology Specialists, SC; Former Section Chief, Assistant Professor, Vascular and Interventional Radiology, Walter Reed Army Medical Center, Uniformed Services University of the Health Sciences
J David Lane, MD, RT is a member of the following medical societies: Alpha Omega Alpha, Society of Interventional Radiology, American College of Radiology, American Heart Association, American Medical Association, American Roentgen Ray Society, Radiological Society of North America
Coauthor(s)
Nick Lomis, MD QI Coordinator, Diagnostic Radiology Service, Assistant Chief, Interventional Radiology and Diagnostic Radiology, Walter Reed Army Medical Center
Nick Lomis, MD is a member of the following medical societies: American College of Radiology, American Roentgen Ray Society, Radiological Society of North America
Specialty Editor Board
Bernard D Coombs, MB, ChB, PhD Consulting Staff, Department of Specialist Rehabilitation Services, Hutt Valley District Health Board, New Zealand
Spencer B Gay, MD Professor of Radiology, Department of Radiology and Medical Imaging, University of Virginia School of Medicine
Chief Editor
John Karani, MBBS, FRCR Clinical Director of Radiology and Consultant Radiologist, Department of Radiology, King's College Hospital, UK
John Karani, MBBS, FRCR is a member of the following medical societies: British Institute of Radiology, Radiological Society of North America, Royal College of Radiologists, Cardiovascular and Interventional Radiological Society of Europe, European Society of Radiology, European Society of Gastrointestinal and Abdominal Radiology, British Society of Interventional Radiology
Zahir Amin, MD, MBBS, MRCP, FRCR Consulting Staff, Department of Imaging, University College Hospital, UK
Zahir Amin, MD, MBBS, MRCP, FRCR is a member of the following medical societies: British Institute of Radiology, British Medical Association, Royal College of Radiologists
References
- Kalliafas S, Ziegler DW, Flancbaum L, Choban PS. Acute acalculous cholecystitis: incidence, risk factors, diagnosis, and outcome. Am Surg. 1998 May. 64(5):471-5. [Medline].
- Shridhar Ganpathi I, Diddapur RK, Eugene H, Karim M. Acute acalculous cholecystitis: challenging the myths. HPB (Oxford). 2007. 9(2):131-4. [Medline].
- Treinen C, Lomelin D, Krause C, Goede M, Oleynikov D. Acute acalculous cholecystitis in the critically ill: risk factors and surgical strategies. Langenbecks Arch Surg. 2015 May. 400 (4):421-7. [Medline].
- D''Agostino HB, vanSonnenberg E, Sanchez RB, et al. Imaging of the percutaneous cholecystostomy tract: observations and utility. Radiology. 1991 Dec. 181(3):675-8. [Medline].
- Flancbaum L, Choban PS. Use of morphine cholescintigraphy in the diagnosis of acute cholecystitis in critically ill patients. Intensive Care Med. 1995 Feb. 21(2):120-4. [Medline].
- Gokhale SM, Lokare S, Nemade P. Role of cholescintigraphy in management of acute acalculous cholecystitis. Indian J Nucl Med. 2012 Oct. 27(4):231-6. [Medline]. [Full Text].
- Kiewiet JJ, Leeuwenburgh MM, Bipat S, Bossuyt PM, Stoker J, Boermeester MA. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology. 2012 Sep. 264(3):708-20. [Medline].
- Adams SD, Blackburn SC, Adewole VA, Mahomed AA. Chronically symptomatic patients with undetectable gall bladder on ultrasonography could benefit from early cholecystectomy. Minim Invasive Surg. 2013. 2013:630753. [Medline].
- Frankel HL, Kirkpatrick AW, Elbarbary M, Blaivas M, Desai H, Evans D, et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part I: General Ultrasonography. Crit Care Med. 2015 Nov. 43 (11):2479-502. [Medline].
- Lakananurak N, Laichuthai N, Treeprasertsuk S. Acalculous Cholecystitis as the Initial Presentation of Systemic Diffuse Large B-Cell Lymphoma. ACG Case Rep J. 2015 Jan. 2 (2):110-2. [Medline].
- Alkhoury F, Diaz D, Hidalgo J. Acute acalculous cholecystitis (AAC) in the pediatric population associated with Epstein-Barr Virus (EBV) infection. Case report and review of the literature. Int J Surg Case Rep. 2015. 11:50-2. [Medline].
- Boland GW, Slater G, Lu DS, et al. Prevalence and significance of gallbladder abnormalities seen on sonography in intensive care unit patients. AJR Am J Roentgenol. 2000 Apr. 174(4):973-7. [Medline].
- Helbich TH, Mallek R, Madl C, et al. Sonomorphology of the gallbladder in critically ill patients. Value of a scoring system and follow-up examinations. Acta Radiol. 1997 Jan. 38(1):129-34. [Medline].
- Molenat F, Boussuges A, Valantin V, Sainty JM. Gallbladder abnormalities in medical ICU patients: an ultrasonographic study. Intensive Care Med. 1996 Apr. 22(4):356-8. [Medline].
Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall.
CT images of emphysematous cholecystitis.
CT cine loop of acalculous cholecystitis demonstrates irregular gallbladder wall, pericholecystic inflammation, and perihepatitis in gallbladder fossa. Necrotic gallbladder was present at surgery.
Normal hepato-iminodiacetic acid scan. Prompt hepatic concentration of radiopharmaceutical is noted, along with early visualization of the gallbladder and drainage into the duodenum.
Hepato-iminodiacetic acid scan of acalculous cholecystitis. Prompt uptake of radiopharmaceutical is noted in the liver, along with drainage into the bowel without gallbladder visualization by 90 minutes.
Ultrasonograms of ICU patient with fever of unclear etiology. Ultrasonographic findings of acalculous cholecystitis include marked gallbladder wall thickening and pericholecystic fluid. Localized tenderness could not be evaluated.
Transverse ultrasonogram demonstrates marked gallbladder wall thickening and pericholecystic fluid collection in a patient with AIDS who was managed conservatively. No localized tenderness was noted, and hepato-iminodiacetic acid scan demonstrated delayed filling but otherwise was normal. Patient recovered with treatment of underlying pneumonia, and ultrasonographic findings normalized within 2 weeks.
A 53-year-old man status post–endoscopic stenting for pancreatic cancer with progressive fever, leukocytosis, and right upper quadrant pain. Ultrasonogram demonstrates gallbladder distension, biliary sludge, borderline wall thickness, and localized tenderness consistent with acalculous cholecystitis.
Image from percutaneous transhepatic cholecystostomy tube placement using coaxial technique demonstrating transhepatic needle access, irregular gallbladder wall, and occluded cystic duct. Note the safety wire adjacent to the definitive 6F drainage catheter.
Despite drainage, this patient continued to experience right upper quadrant pain and leukocytosis. Ultrasonographic and CT scan studies demonstrate transhepatic cholecystomy catheter in good position, but interval development of markedly worsening gallbladder wall edema and pericholecystic inflammatory changes have occurred. At surgery, gangrenous gallbladder was found and resected successfully.
Ultrasonographic images from percutaneous cholecystomy using the trocar technique. Ultrasonography guides transhepatic access to the gallbladder with a 6F trocar drainage catheter. After access, the catheter is fed forward to reform the distal pigtail within the gallbladder lumen and is locked in this configuration.
Cine image of pigtail catheter moving freely within the gallbladder, which confirms adequate placement, along with free return of bile from the catheter.
Cine loop percutaneous cholecystostomy tractogram demonstrates immature tract 3 weeks after percutaneous cholecystostomy. Free spillage of contrast into the peritoneal space is noted. Drainage was continued for an additional 2 weeks prior to catheter removal.
Cholecystogram 4 weeks status post–cholecystomy tube placement for acalculous cholecystitis demonstrating a patent cystic and common duct and the absence of calculi. All clinical signs and symptoms had resolved.
